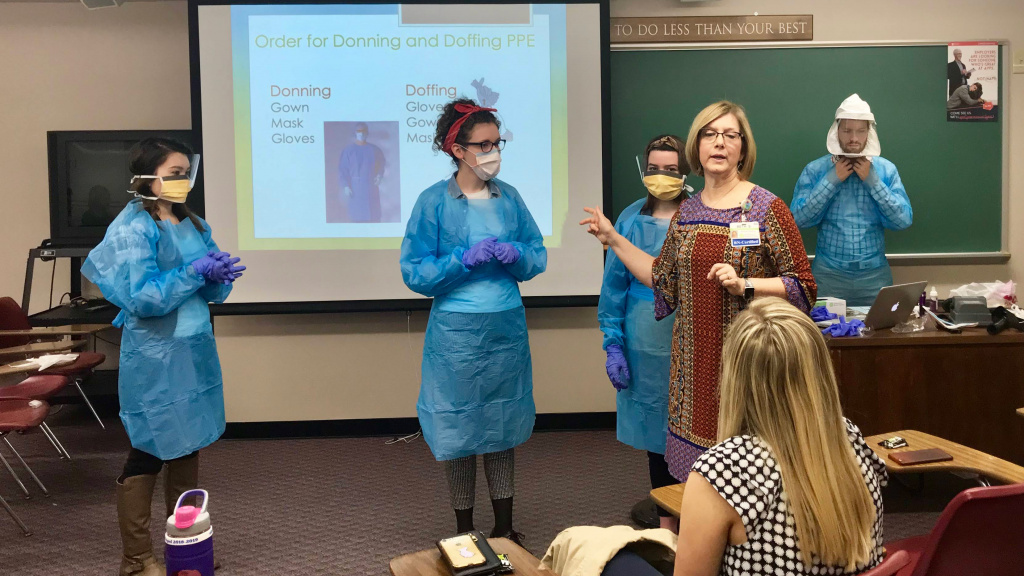
The following interview with Beth Smith (Class of ’88) was submitted by Melanie Schell, Class of ’84 and professor in BJU’s Division of Health Sciences. Because Schell couldn’t ask Smith to be a guest speaker in her epidemiology class, she asked her to answer questions via email. Smith works as an infection control specialist in Greenville, South Carolina. The attached photo is from one of Smith’s previous guest speaking appearances in epidemiology.
What has been the most significant change in hospital protocol, that in your mind has had the biggest effect on transmission rates (of COVID-19 and/or other infectious agents)?
For COVID-19, we have implemented universal masking. This means that anyone who enters the hospital is screened at the door for fever or respiratory illness. If sick, they are given a mask and not permitted to enter (unless it is a patient here for treatment). If they pass the screening, they are given a mask to wear for their shift. A different mask would be worn (and discarded after use) if they go into an isolation room.
This practice of universal masking reduces the risk of transmission to our team members from undiagnosed and/or asymptomatic patients as well as transmission from a team member to a patient. We eliminated potential visitor transmission risk by restricting visitors to end-of-life visitation. That was a difficult but necessary decision that has been nationally implemented by most hospitals. For now, we are using a hospital-provided face mask but will look at cloth masks if we exhaust our face mask supply.
What, if any, changes do you think will be permanent changes at Prisma?
Most of the infection prevention measures are unique to this pandemic (such as) allowing a single-use mask to either be reprocessed as well as be worn for an entire shift. (They are) not practices that we would endorse when resources are available. Cohorting of isolation patients to specific floors is also a practice that is resourceful for this pandemic but not practical for our normal operations.
What we have found is that technology like Skype prior to this have been underutilized. In our need to avoid groups, Skype has become an invaluable tool that I believe we will continue to utilize. We use a lot of time trying to gather people together from across the campus when Skype is much more time efficient.
We have seen an increase in our hand hygiene compliance. I would hope that this is a permanent change. There was a lot of distrust that the data was accurate, but with this virus we can show the rise in hand hygiene as team members are cleaning their hands more. The reality is that we clean our hands more when we have a fear of transmission of disease to ourselves.
Has Prisma been affected by the lack of PPE? How have those issues been handled by the front line professionals?
Absolutely! We have used multiple resources to get face masks and N95 respirator masks. We have an Incident Command Center meeting every morning with one of the reports detailing what the number of masks on hand is and with our projected use (“burn rate”), how many days it will last us.
Additionally, (we) have begun using Bioquell (vaporized hydrogen peroxide) to reprocess used N95 masks. These reprocessed masks are not currently being used but are being stockpiled in case we deplete our current inventory. There is a lot of uncertainty among team members to consider using a reprocessed mask, but if it comes to a mask that has been tested to show its safety (Clemson is helping with that testing) or not having a mask, I believe they would choose to use this mask. My hope is that we will not need to use them but am grateful to have a fallback option.
Why did Prisma change their approach from identifying employees who had been exposed to COVID-19 to testing based on their symptoms?
With the implementation of universal masking, the CDC-defined exposure risk of team members to COVID-19 was reduced to a low risk. This risk level only requires that team members monitor for symptoms of illness — fever, cough, shortness of breath, sore throat — and are tested if they do become ill.
What are your thoughts on how a Christian health care professional should view these circumstances? Any verses that you have claimed to keep you going?
There have been so many situations in which I’ve had to deal with team members who are so fearful. This fear is primarily from lack of understanding of how transmission can be prevented and their concern that they will “take it home” to their loved ones. (The fear I have seen is similar to the HIV/AIDS epidemic in the 1980s, but we were not limited in our PPE in providing for that population as we are now.) I have had to ask God for wisdom in dealing with these many situations. They needed fact and compassion. I have had to help with a former coworker who had a dying family member hospitalized and the visitation restrictions did not allow her to visit. She was not immediate family. God allowed me to pray with this friend over the phone. I don’t always get an opportunity to give a clear witness, but when they consent to allowing me to pray with them, they get it.
The first week that COVID-19 hit the Upstate, my pastor emailed me Psalm 91:1–6. I have meditated on these verses often since then. It is such a comfort to know that we can abide in the shelter of the Almighty, even in the midst of a pandemic. The image of Christ sheltering us beneath His wings so that we need not be afraid was not just beautiful imagery but became a source of reassurance that I need not fear but to trust in Christ.
And one additional verse to share: Isaiah 26:3, which reminds us that God is our source of peace in the midst of our hardest days.

Beth Smith
Class of ’88