“Three and a half years ago, my voice was all I had. That’s all I thought I had to offer. Little did I know the journey God was about to take me on that would prove that statement as wrong as it could be.”
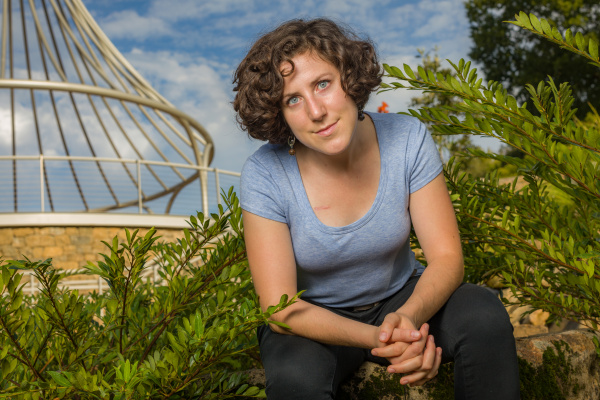
Dr. Shellie Beeman, BJU alumna and vocal studies department head, wrote her doctoral dissertation on voice injuries and has two certifications in the care and the health of the voice. “And yet,” she said, “my voice broke down. I didn’t even have a voice.”
A Lost Voice
In January 2017, Beeman was preparing for a recital when she started losing the top of her vocal range. “I had completed a fabulous recital rehearsal the day before, only to wake up the next day without the top of my range,” she said.
Beeman continued to lose notes over the next few days before she called her doctor, who referred her to an ear, nose and throat specialist. “I went to see the ENT-PA … and she did what they call a basic scope. It’s not the fancy strobe. It’s just stick the camera up your nose, down your throat, (and) take a look.”
The ENT told Beeman after the procedure that she had seen a bit of swelling and minor pre-nodules. “Just waterworks right there,” recalled Beeman. “How did this happen? … The parts weren’t all connecting. I hadn’t done anything to warrant even pre-nodules”
Yet Beeman determined to follow the doctors’ orders without questioning. “I put aside everything I knew, all the expertise I had, in my determination to be a good client. I committed to ‘I’m not going to ask questions. I’m going to be a good client because I want to get better. All I want is my voice back, so I’m just going to do this,’ ” she said.
Beeman’s ENT-PA referred her to a Speech-Language Pathologist for voice therapy. After spending February through May in different therapies and a summer of rest and light voice practice, Beeman saw slight improvement. However, in August, she relapsed and lost more of her voice than she had before. “Where I at least had a high A5 after therapy, now I could not sing above a D5, and very badly at that,” she said. “I barely had an octave, and it was very effortful and very painful to sing. My speaking voice while teaching just always hurt.”
From February to May 2017 as Beeman did her voice therapy and worked with the medical professionals, the one issue no one could solve was her neck pain. “It always came back to my neck just hurts. It’s hurting. (My Speech-Language Pathologist) couldn’t figure it out, so she sent me to my chiropractor. He ended up doing some adjusting, but also some muscle release techniques. But I would get about 24 hours out of it, and then it would go back to hurting.”
A Difficult Journey
At this point, Beeman’s medical team had advised her to reduce how much she used her voice. “I had been asked to reduce my speaking,” she said. “I didn’t go to church for three months because (they told me), ‘You can’t afford to socialize. You just need to go home.’ I stopped going to friends’ houses. I stopped calling family members. It was a very miserable time of my life. No interaction, just kind of barely making it. For the first time in my life, I wasn’t just lonely. I was alone — lost.”
There were moments when Beeman wondered if she would need to consider a new career path. “I literally cannot sing, and I can barely talk.” How could she teach students to use their voices when she couldn’t?
“Going through the loneliness. Being asked to not go to church for three months. Reducing how much I was speaking. Something my doctors insisted on is that I not take work home — which sounds really nice, except my daytime hours are very full,” Beeman said.
“Here I was, three degrees in voice, a secondary emphasis in Speech-Language Pathology, two vocal certifications, and a dissertation on vocal health. My voice wasn’t supposed to break down, but it did. For a while, I looked for people to blame, including God. I did not realize how much of my identity as a person was in my singing and in my teaching. Simply put, I WAS my career, and my career was ME.
“I have since come to learn that I am more than my career and that often, God entrusts us with negative experiences so that we can later help others. I think of the students who have come through my studio, and how much better I can now affect their lives, vocally, physically, emotionally and spiritually.”
A Bold Determination
The September after Beeman’s relapse in August 2017, her ENT clinic hired a new laryngologist who specialized in the voice. Beeman recalled the first appointment, “He looked at me and very honestly said, ‘I don’t know why this is happening. You’ve done everything. You’ve done it all right.’ I was stunned at the humility of this doctor!”
Beeman says it was at that moment that she realized her situation was not a vocal overuse or nodule situation. “Because had it been nodules, it would have gotten better.”
After attempting some additional voice therapy and training, Beeman met again with her new ENT in December. “But this time he thought he actually saw a paresis, which is (when) one vocal fold is paralyzed. And once again my checklist is just running, going, ‘But I haven’t done anything (to cause a paresis).’” They decided to continue another three months with the current plan to see if there would be any improvement.
When Beeman went into her March appointment, she told her ENT and the head SLP at Greenville Health System ENT, “Something in my body is telling me I can sing. I can’t explain it to you, but my body wants to sing, but something is keeping me from singing, and I need to know what it is. I refuse to believe that it cannot be fixed.” The ENT referred her to his mentor, Dr. Thomas Cleveland, in Nashville, Tennessee, at the Bill Wilkerson Voice Clinic.
A Recovered Hope
Dr. Cleveland asked Beeman about her entire history, going back further than the initial onset of this incidence of pain. “We talked through the whole thing up to that point,” said Beeman. Then, they went to strobe Beeman’s vocal folds.
“He’s got a computer screen right there where I can see the whole thing. … And I kid you not, I had never seen a more beautiful pair of vocal folds,” Beeman said.
Beeman and Dr. Cleveland went back to the exam room, with Beeman’s mind a whirl of questions. When they arrived, the doctor asked Beeman to sing.
“It was terrible,” said Beeman. “When I say it was terrible, my voice by this time was very gruff, very rough, very wobbly. I had no control over the vibrato. I couldn’t sing above a D5. It was painful to me, and it just hurt.”
Dr. Cleveland did some adjusting and massaging of Beeman’s throat, then asked her to sing again, asking if it felt different. It did. “And he literally just grinned at me,” Beeman said.
The doctor diagnosed Beeman with — not a paresis, not nodules, not reflux — stress-induced muscle tension dysphonia.
When Beeman graduated with her master’s degree from BJU in 2006, she went to Chicago to begin a career in performance. Then, she took a job teaching at a college in Wisconsin which resulted in what Dr. Cleveland believed was a traumatic turning point in Beeman’s career and vocal health. She went on to doctoral school at Ball State, then took a job in Colorado, where she was mistreated for her faith. When she joined the faculty at BJU in 2016 and began with a larger load, “it was just the straw that broke the camel’s back,” she said.
Dr. Cleveland believed Beeman’s injury went back to 2009–2010. “I’m an introvert, so I internalize everything.” Beeman explained, “What actually happened, (wasn’t in the vocal folds), it was all of these muscles in my back and shoulders that just took over, and that’s why I had so much pain.”
The Road Back
Beeman came back to Greenville armed with exercises and on the hunt for new therapists. “I was in therapy three times a week,” she said. “It was a very specific kind of therapy — physical therapy, manual therapy and Myofascial Release therapy.”
After completing therapy, Beeman still had some pain and vocal fatigue. At the recommendation of her Christian Speech-Language Pathologist, she contacted her pastor for counseling and a local voice teacher to retrain her voice.
“We met for a first lesson in November of 2018, and I explained everything to him,” Beeman said. “So, he had me sing and said, ‘I want you to do this. I want you to actually not think about singing, just do it.’ I was really scared because he was asking me to basically use my voice more. Well, I hadn’t done that in two years. So, I did it, and somehow, he got me up to a very high D6. I had not sung that in a year and a half.”
In the early spring of this year, Beeman asked her teacher about doing a recital. His answer: “Yeah! You just need to sing!” Though now in her third year of physical therapy, Beeman’s first full recital since her injury will be at 7 p.m. on Saturday, Sept. 26 in War Memorial Chapel.
“The way that I like to describe what happened to me,” said Beeman, “it’s like going through a grieving process. It’s like a part of me died. And having to mourn those things and work through it but being thankful to God that I came out on the other side because I think He wanted me to. He had a purpose for me, and I truly believe I’m a better teacher and a better person.
“God had things for me to learn, and I think I’m still learning. I don’t think this whole thing is done. It doesn’t feel done yet. It’s been a journey, but I still have so much more to learn. And I think those of us that can now relate to the chronic pain, the loss, the identity crisis — it changes you. Significantly.”
Dr. Beeman and Dr. Lorri Turcios, pianist, collaborate for “Finding My Way Back through French Song.” Student, faculty and staff tickets are available.