Even after living almost a year through a global pandemic, many still have questions about COVID-19. Dr. Bernard Kadio — School of Health Professions professor, population health scientist and director of BJU’s Center for Community and Global Health — provides answers.
Is COVID-19 real and is it that serious? Are we not giving in to too much fear as Christians?
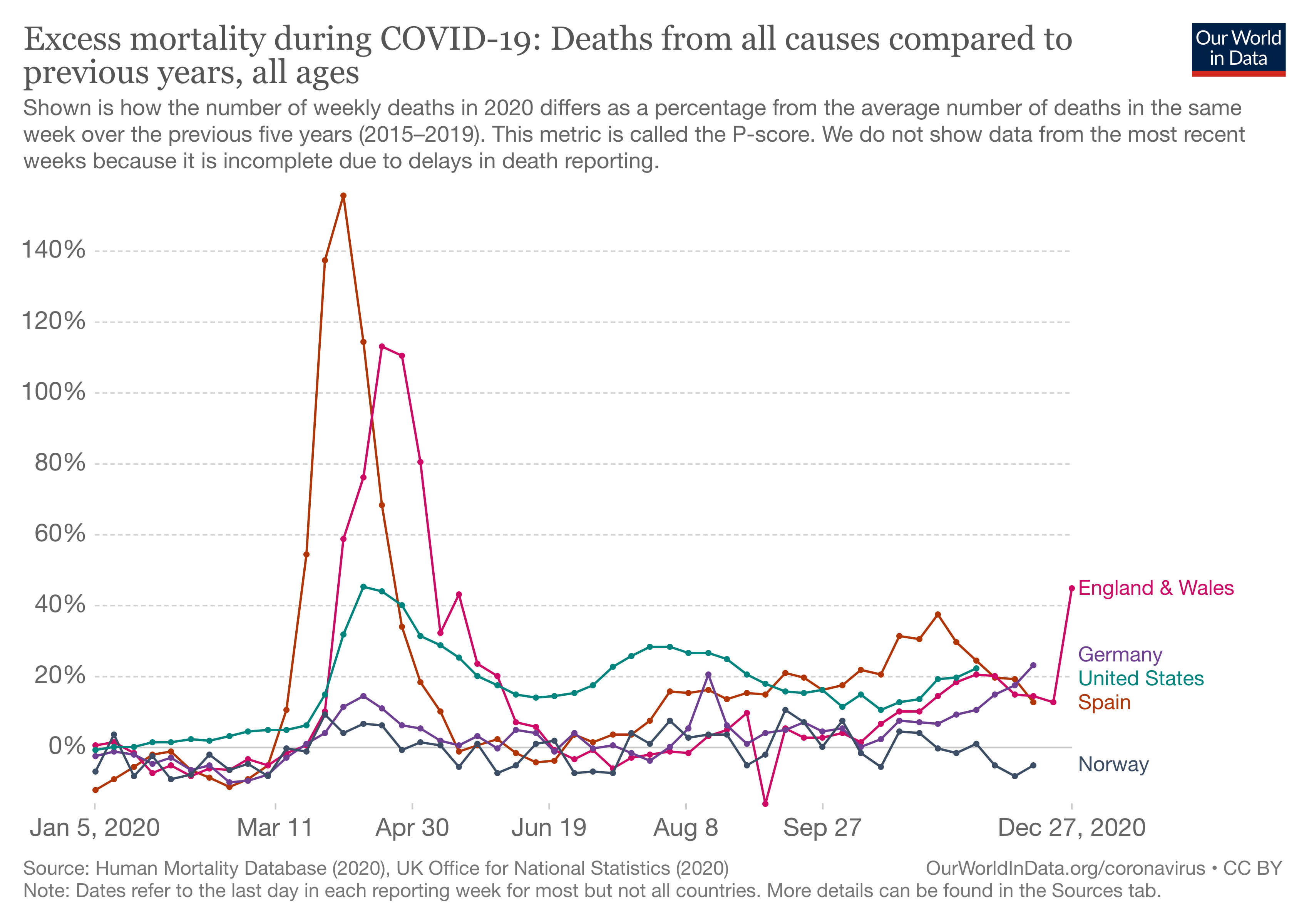
Recent US epidemiological data suggest that COVID-19 is quickly changing the mortality profile of the nation. By October 2020, the pandemic was among the leading causes of death, only third to heart diseases and cancer.[1] In December 2020 the mortality rate by COVID-19 surpassed cancer making the pandemic the second cause of death in the country. Daily mortality rates for heart disease and cancer, which for decades have been the two leading causes of death, are approximately 1,700 and 1,600 deaths per day, respectively.[2] Similarly, most European countries recorded an excess mortality in the year 2020 due to the pandemic.[3]
Some question the validity of the COVID-19 numbers arguing a malicious exaggeration. While it’s to be noted that no epidemiological data reporting system is perfect, it’s hard to believe that the entirety of the health systems around the country and around the globe would systematically and unethically falsify their data, breaching their long-established traditional reporting protocols. An indirect proof of the seriousness of the disease would be to consider the fact that at this point in the pandemic, we all know someone who has been near to dying or someone who has succumbed to the disease.
Also, for believers to use protective measures is not an indicator of fear but of wisdom. Using an umbrella when it’s raining or a coat when it’s cold doesn’t mean that you do not believe that our Lord can heal pneumonia.
Do face masks really work? Are they not a political attempt to limit our freedom?
An analysis of patient safety in medical and surgical practices and in the protection of healthcare professionals against hospital-acquired infections quickly reveals two major discoveries that have changed the face of medical and surgical practices around the globe. Both discoveries happened over 100 years ago. First, Ignaz Semmelweis, a Hungarian doctor who worked at the Vienna General Hospital between 1844 and 1848, evidenced that the death of mothers due to postpartum sepsis was significantly reduced in-unit when and where OB-GYN doctors practiced appropriate handwashing.[4] In spite of the tremendous technological advancement of our century, appropriate handwashing remains one of the most critical behaviors to prevent germ transmission, not only in hospital settings but also in personal hygiene.
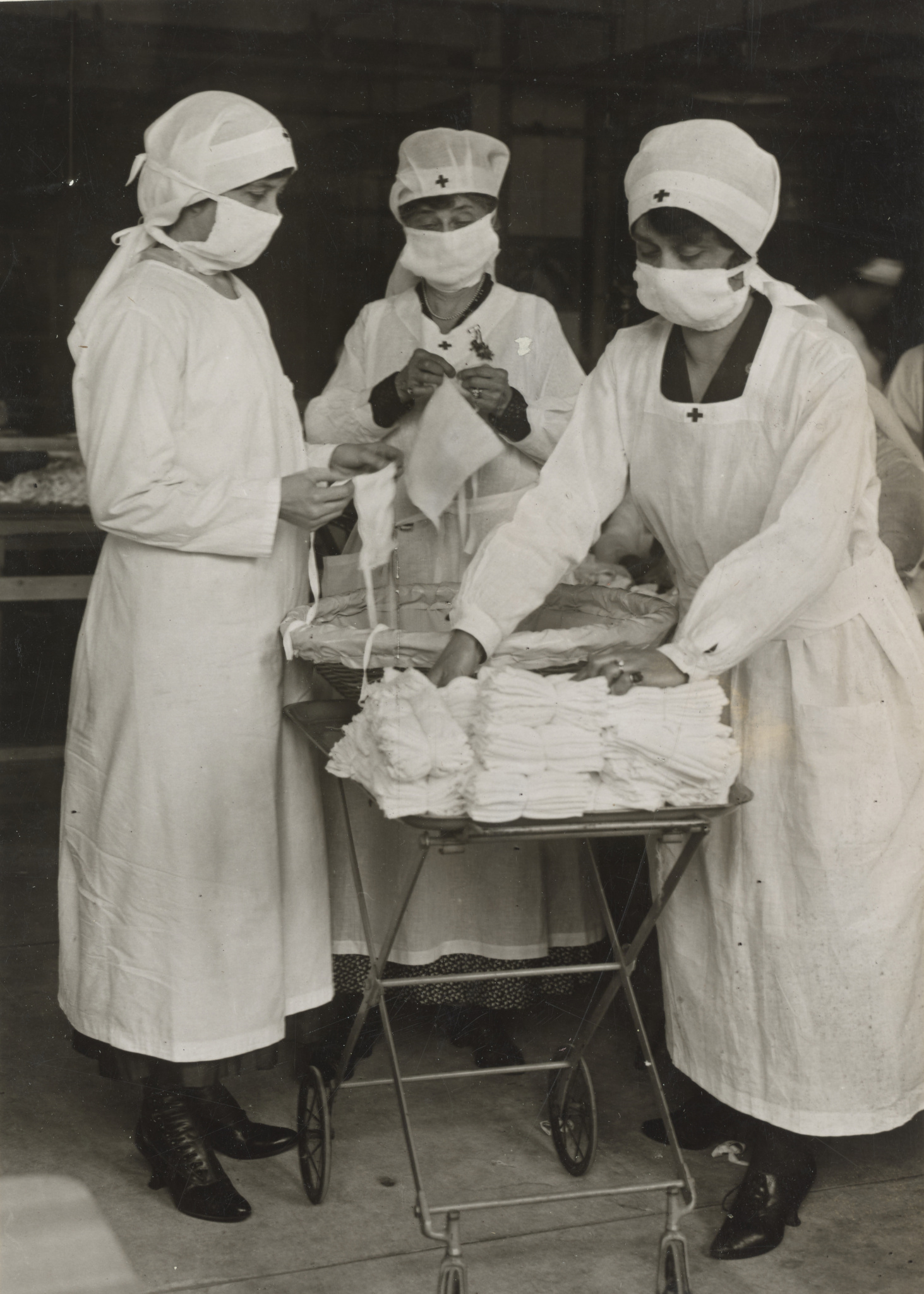
Secondly, in 1880 Johann Mikulicz, head of the surgery department at the University of Breslau (now Wroclaw, Poland), and bacteriologist Carl Flügge, who had shown that respiratory droplets carry culturable bacteria, started wearing face masks during surgery. These masks were described as “a piece of gauze tied by two strings to the cap, and sweeping across the face so as to cover the nose and mouth and beard.”[5] As a result of their experience, the use of face masks and other surgical gowns became gradually widespread in Europe and the U.S. by the beginning of the 20th century. If PPEs and face masks are able to protect against the transmission of germs in complex and highly exposed clinical settings, their efficacy in preventing community spread during respiratory outbreaks is quickly understood. Thus, they became essential in stopping the Manchurian plague in 1910–11 and a decade later the deadly 1918–1919 influenza pandemic.
I have already been infected last semester. Should I still observe the public health measures?
Respiratory infections due to endemic or seasonal coronaviruses provide a certain degree of immunity in the general population, especially in young children although that immunity is short-lived.[6] However, for epidemic coronaviruses such as SARS-CoV-1, MERS and SARS-CoV-2, there is insufficient data at this point to support a long-term immunity claim.
Another complicating factor is that there are several variants of the virus in circulation due to mutations, and there’s no data to back a crossed immunity between the different strains. Although after 12 months of the current pandemic the number of true reinfections remains extremely low compared to the number of cases, a public health approach would recommend prudence in absence of established evidence.
It’s therefore advised to maintain the 4 W’s even if one has been previously exposed to the virus, especially when in a community setting.
Can we even trust the new vaccines?
Advances in genomics and gene technologies over the last two decades have increased our understanding of viruses and viral infection. Consequently, the approach to vaccines has also been revolutionized. The trend is now toward precision vaccination in which a specific molecular structure of the pathogen is injected in lieu of the entire live-attenuated or the inactivated pathogen, like for example the polio vaccines (OPV and IPV).
One of the key advantages of the new technologies is that safety and efficacy concerns are lessened because of the use of minimally invasive materials since no adjuvant nor stem cells are needed.[7] The other gain is time, which is critical in the context of a pandemic. The gene technologies allow faster development of vaccines.
The current COVID-19 vaccines are centered on Protein S (Spike protein) and nucleic acid fragments (mRNA). Viral vectors and protein synthesis are the viral technologies used.
The FDA has issued an Emergency Use Authorization meaning preliminary data suggest a certain degree of safety and efficacy. Nonetheless, as with any vaccine, extreme caution should be exercised in individuals with a history of allergies and focus should be placed on individuals who are constantly exposed to the virus or who are likely to develop fatal outcomes if they were to contract the disease.
When will all this be over?
The 1918 Influenza Pandemic lasted for two to three years depending on the country (1918–1920). The 2003 SARS-CoV-1 epidemic lasted approximately eight months. The 2012 MERS outbreak never developed into a full pandemic. We don’t know the full extent of the intimate mechanisms that determine the circulation of new pathogens in humans. Herd immunity is certainly a key, but other environmental parameters are also at play.
For believers, a vertical aspect should also be considered. The historic role of Christians in Rome during the Justinian Plague (541–543) sets a framework of the Christian attitude in times of calamity: love, prayer and engagement instead of rejection and retreat.
From a public health perspective, it’s important to have a system in place to monitor the spread of the virus, for example, a traffic light system that will inform decision-makers when to remove public health measures. Such a system on campus would be beneficial as it could help prevent what has been described as “COVID-19 fatigue” and contribute to a profitable social experience on campus.
[1] https://jamanetwork.com/journals/jama/fullarticle/2774465
[2] https://wonder.cdc.gov/ucd-icd10.html
[3] https://ourworldindata.org/excess-mortality-covid
[4] Loudon, I. (2013). Ignaz Phillip Semmelweis’ studies of death in childbirth. Journal of the Royal Society of Medicine, 106(11), 461-463.
[5] Strasser, B. J., & Schlich, T. (2020). A history of the medical mask and the rise of throwaway culture. The Lancet.
[6] Edridge, A. W., Kaczorowska, J., Hoste, A. C., Bakker, M., Klein, M., Loens, K., … & van der Hoek, L. (2020). Seasonal coronavirus protective immunity is short-lasting. Nature medicine, 26(11), 1691-1693.
[7] Afrough, B., Dowall, S., & Hewson, R. (2019). Emerging viruses and current strategies for vaccine intervention. Clinical & Experimental Immunology, 196(2), 157-166.